Abstract
Background: Despite major improvements in survival, relapse is still a frequent and severe event in pediatric acute myeloid leukemia (AML). Cytogenetic abnormalities represent important predictors of outcome. Improved risk stratification encompassing the identification of novel cytogenetic subsets may allow refinements in treatment strategies and increase survival rates.
Hypodiploidy, defined as a modal number (MN) below 46 chromosomes, is associated with an adverse outcome in pediatric acute lymphoblastic leukemia. In childhood AML, the predominant cause of hypodiploidy is loss of a sex chromosome accompanying t(8;21). The most commonly lost autosome is chromosome 7, associated with a poor prognosis. However, other chromosome losses in pediatric AML have not been independently explored.
We aimed to investigate the occurrence, genetic characteristics, and prognostic impact of hypodiploidy in childhood AML.
Methods: This study was conducted as a retrospective cohort study within the I-BFM-AML framework. Children 0-18 years of age diagnosed with de novo AML between January 2000 to December 2015 and a hypodiploid karyotype were eligible for inclusion. Patients with constitutional hypodiploidy, monosomy 7, composite karyotypes, and t(8;21) with loss of a sex chromosome were excluded.
Cytogenetic review was performed according to International System for Human Cytogenetic Nomenclature. Hypodiploidy was considered clonal when occurring in at least three metaphases. The clone with the lowest MN defined the ploidy level. The log-rank test was applied for estimating difference in survival. Considering allografting in first complete remission (CR1) as a time-dependent event, the effect of stem cell transplantation (SCT) on overall survival (OS) was estimated by the Mantel-Byar method. Multivariate analyses included sex, complex karyotype (≥3 non-recurrent aberrations), FLT3-ITD mutation status, and white blood cell count as covariates. As all patients with FLT3-ITD mutations had same MN (MN=45) leading to a skewed imputation model, multiple imputation was not performed, and multivariate analyses included complete cases only (n=54).
Results: Hypodiploidy was detected in 81/6,409 patients with full karyotyping from 14 collaborative study groups, yielding a frequency of 1.2% in childhood AML. The cohort displayed a balanced sex distribution (male/female: 42/39) and a median age of 6 (range: 0-17). MNs 45 (n=66), 44 (n=10) and 43 (n=5) were observed. No patient had MN below 43. Eight patients (9.8%) had chromosome loss as the only aberration. Forty-eight patients (59%) had a complex karyotype. Core-binding factor abnormalities were observed in three patients (3.7%). Four patients harbored FLT3-ITD mutations (9.3%, 54 tested).
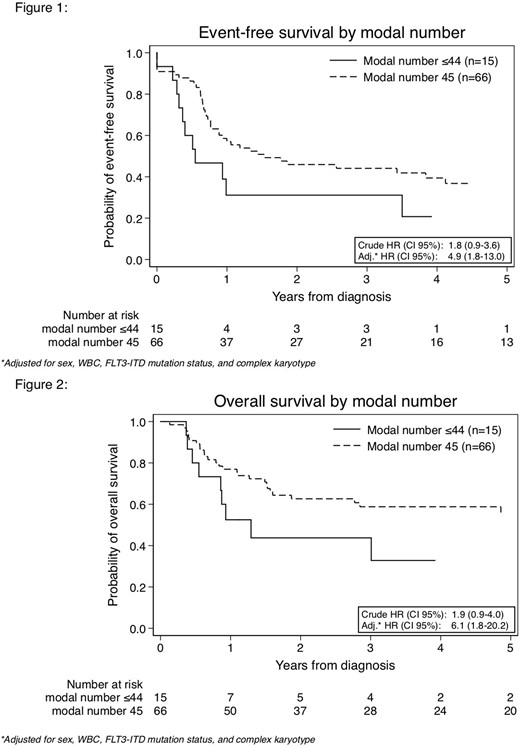
Median follow-time for patients alive was 4.5 years (range: 0.2-15.3). Five-year event-free survival (EFS) and OS were 34% (CI 95%: 23% - 45%) and 52% (CI 95%: 40% - 63%), respectively. Cumulative incidence of relapse was 50% with a median time-to-relapse of 0.8 years. Twelve out of 38 relapsed children (32%) were alive at the end of follow-up. Children with MN≤44 (n=15) had lower EFS (21%, CI 95%: 4% - 46%) and OS (33%, CI 95%: 10% - 59%) than children with MN=45 (n=66, EFS: 37%, CI 95%: 24% - 49%, OS: 56%, CI 95%: 42% - 68%). Crude hazard ratios (HR) for MN≤44 vs MN=45 were 1.8 (p=0.08) for EFS and 1.9 (p=0.1) for OS. After adjustment HRs increased to 4.9 (p=0.001) and 6.1 (p=0.003), respectively. Loss of chromosome Y (n=12) displayed a non-significant superior survival (EFS: 58%, OS: 75%). Poor survival rates were especially observed in monosomy 9 (n=11, EFS: 14%, OS 15%), 10 (n=5, EFS: 20%, OS: 20%), and 16 (n=5, EFS: 25%, OS: 25%), although not reaching statistical significance.
Allogenic SCT did not offer any advantage in survival. For children receiving SCT in CR1 (n=18), crude HR for OS was 1.4, p=0.39. Multivariate analysis showed HR for OS at 1.5, p=0.42. Exclusion of children not reaching CR1 (n=7) did not significantly change HRs.
This large international study reveals that hypodiploidy is rare in pediatric AML. Children with loss of chromosome 9, 10, or 16 all displayed unfavorable survival rates, whereas loss of chromosome Y did not have influence on prognosis. SCT in CR1 did not improve survival. Our results suggest that modal number has an impact on outcome and may be important for risk stratification.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.